Machine Learning in Healthcare Transforming Patient Care
Discover how machine learning in healthcare revolutionizes patient care through AI diagnostics, predictive analytics, personalized treatment plans

The healthcare industry stands at the precipice of a revolutionary transformation, driven by the unprecedented integration of machine learning in healthcare. This technological evolution is fundamentally reshaping how medical professionals diagnose diseases, develop treatment protocols, and deliver patient care. As we navigate through 2025, artificial intelligence and machine learning algorithms have transcended their experimental phases to become indispensable tools in modern medical practice, offering solutions to longstanding challenges that have plagued healthcare systems for decades.
Machine learning, a subset of artificial intelligence, empowers computers to learn from vast datasets without explicit programming, enabling them to identify patterns, make predictions, and continuously improve their performance over time. In healthcare settings, this capability translates into transformative applications ranging from early disease detection and medical imaging analysis to personalized medicine and predictive analytics. The convergence of big data, advanced computational power, and sophisticated machine learning techniques has created an ecosystem where healthcare providers can make more informed decisions, reduce diagnostic errors, and ultimately save lives.
The impact of machine learning in healthcare extends far beyond technological novelty. It addresses critical pain points, including physician burnout, through AI-powered clinical decision support systems, improves patient outcomes through precision medicine, and enhances operational efficiency through predictive healthcare analytics. Electronic health records (EHR) now serve as rich data sources for machine learning models, enabling real-time patient monitoring and risk assessment that were previously impossible.
As deep learning and natural language processing continue to advance, the potential applications multiply exponentially. From drug discovery accelerated by artificial intelligence to remote patient monitoring enabled by wearable health devices, the healthcare landscape is witnessing unprecedented innovation. This comprehensive exploration delves into how machine learning is not merely augmenting but fundamentally transforming patient care delivery, examining both its remarkable achievements and the challenges that must be addressed to realize its full potential in creating a more efficient, accessible, and effective healthcare system for all.
Machine Learning in the Healthcare Context
Machine learning in healthcare represents a paradigm shift in how medical data is processed, analyzed, and utilized for clinical decision-making. At its core, machine learning involves training algorithms on large datasets to recognize patterns and make predictions without being explicitly programmed for specific tasks. In the healthcare domain, this translates to systems that can analyze patient information, medical images, genomic data, and clinical records to provide actionable insights that support healthcare providers in delivering superior patient care.
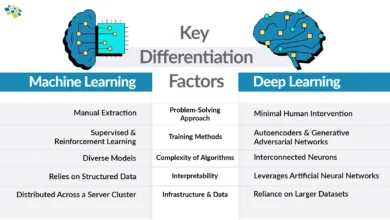
The foundation of machine learning rests on three primary learning approaches. Supervised learning uses labeled datasets to train models for specific tasks like disease diagnosis and patient risk stratification. Unsupervised learning identifies hidden patterns in unlabeled data, proving valuable for discovering disease subtypes and patient segmentation. Reinforcement learning enables systems to learn optimal treatment strategies through trial and error, showing promise in treatment planning and personalized therapy recommendations.
Deep learning, a sophisticated subset of machine learning, utilizes artificial neural networks with multiple layers to process complex data. In healthcare, deep learning models excel at analyzing medical imaging data, including X-rays, MRIs, and CT scans, often achieving accuracy levels comparable to or exceeding human radiologists. Convolutional neural networks (CNNs) have become particularly effective for image recognition tasks, while recurrent neural networks (RNNs) process sequential data like electronic health records and time-series physiological measurements.
The integration of natural language processing allows machine learning systems to extract meaningful information from unstructured clinical notes, research papers, and patient-reported outcomes. This capability bridges the gap between human communication and machines, enabling more comprehensive analysis of patient histories and medical literature. Predictive analytics powered by machine learning can forecast disease progression, hospital readmission rates, and treatment responses, empowering healthcare professionals to intervene proactively rather than reactively.
The successful implementation of machine learning in healthcare requires robust data infrastructure, including standardized electronic health records, secure data sharing protocols, and high-quality annotated datasets for training machine learning models. As these foundational elements mature, the accuracy and reliability of AI-driven healthcare solutions continue to improve, paving the way for widespread adoption across diverse clinical settings.
Early Disease Detection and Diagnosis
Early disease detection represents one of the most impactful applications of machine learning in healthcare, offering the potential to identify conditions before they progress to advanced stages. Machine learning algorithms analyze multiple data sources simultaneously, including medical imaging, laboratory results, genetic markers, and patient histories, to detect subtle patterns indicative of disease that might escape human observation. This capability is particularly transformative for conditions where early intervention dramatically improves outcomes, such as cancer, cardiovascular disease, and neurodegenerative disorders.
In oncology, machine learning models have demonstrated remarkable proficiency in identifying malignancies from medical imaging data. Deep learning algorithms trained on millions of mammograms can detect breast cancer with accuracy rates exceeding 90%, sometimes identifying tumors that radiologists initially missed. Similarly, computer vision techniques applied to skin lesion images can distinguish between benign and malignant melanomas with dermatologist-level accuracy, making early cancer detection more accessible and cost-effective.
Cardiovascular disease prediction has been revolutionized through machine learning analysis of electrocardiogram (ECG) data, echocardiograms, and patient risk factors. Predictive models can identify individuals at high risk for heart attacks or strokes years before clinical symptoms manifest, enabling preventive interventions such as lifestyle modifications or pharmacological treatments. Artificial intelligence systems continuously monitor wearable device data to detect irregular heart rhythms, including atrial fibrillation, alerting patients and physicians to potential dangers in real-time.
Diabetic retinopathy, a leading cause of blindness, exemplifies how machine learning democratizes specialized care. AI-powered diagnostic systems can screen retinal images for signs of diabetic eye disease with ophthalmologist-level accuracy, making screening accessible in primary care settings and underserved communities where specialist availability is limited. Google Health and other technology companies have developed deep learning models that analyze retinal photographs to detect not only diabetic retinopathy but also cardiovascular risk factors, demonstrating the multi-faceted diagnostic potential of AI in healthcare.
Neurological conditions, including Alzheimer’s disease and Parkinson’s disease, benefit from machine learning analysis of brain imaging, speech patterns, and movement data. Predictive analytics can identify cognitive decline years before clinical dementia diagnosis, opening windows for therapeutic intervention and clinical trial enrollment. Machine learning algorithms analyzing patient symptoms, genetic profiles, and biomarkers are accelerating the identification of rare diseases, reducing the diagnostic odyssey that patients with uncommon conditions often endure.
The integration of genomic data with machine learning has enabled precision medicine approaches to disease detection. AI systems can identify genetic mutations associated with cancer predisposition or rare inherited conditions, facilitating preventive monitoring and early therapeutic intervention. As machine learning models are trained on increasingly diverse and comprehensive datasets, their ability to detect diseases across different populations and presentations continues to improve, addressing historical biases in medical research and practice.
Predictive Analytics for Patient Outcomes
Predictive analytics powered by machine learning has transformed how healthcare systems anticipate and manage patient outcomes, shifting the paradigm from reactive to proactive care. By analyzing historical patient data, treatment patterns, and clinical variables, machine learning models can forecast disease progression, treatment responses, and potential complications with unprecedented accuracy. This predictive capability enables healthcare providers to allocate resources efficiently, personalize interventions, and improve overall patient care quality while reducing costs.
Hospital readmission prediction represents a critical application of predictive analytics in healthcare. Unplanned readmissions burden patients, strain healthcare systems, and indicate suboptimal care quality. Machine learning algorithms analyze electronic health records, including diagnosis codes, medication lists, laboratory values, and social determinants of health, to identify patients at high risk for readmission within 30 days of discharge. These predictions enable care teams to implement targeted interventions such as enhanced discharge planning, home health services, or close outpatient follow-up, significantly reducing readmission rates.
Sepsis prediction exemplifies the life-saving potential of predictive machine learning in acute care settings. Sepsis, a systemic inflammatory response to infection, progresses rapidly and carries high mortality if not treated promptly. AI-powered early warning systems continuously monitor patient vital signs, laboratory results, and clinical data from electronic health records to identify subtle patterns indicative of developing sepsis hours before clinical recognition. This early detection enables timely antibiotic administration and intensive care interventions, dramatically improving survival rates.
Intensive care unit (ICU) patients benefit significantly from predictive analytics that forecast deterioration, complications, and mortality risk. Machine learning models trained on physiological data from bedside monitors, ventilator settings, medication administration records, and laboratory results can predict acute kidney injury, ventilator-associated pneumonia, and cardiac arrest with lead times sufficient for preventive action. These predictions help critical care teams prioritize interventions and optimize resource allocation in high-acuity environments.
Chronic disease management leverages predictive analytics to identify patients likely to experience exacerbations or complications. For diabetes patients, machine learning models predict hypoglycemic events based on continuous glucose monitor data, insulin dosing, physical activity, and dietary patterns, enabling timely preventive measures. Similarly, patients with heart failure benefit from predictions of decompensation based on wearable sensor data, weight trends, and symptom reports, facilitating early intervention before hospitalization becomes necessary.
Treatment response prediction represents another frontier for predictive machine learning in personalized medicine. By analyzing patient characteristics, biomarkers, and historical treatment outcomes, AI systems can forecast which therapies are most likely to succeed for individual patients. In oncology, predictive models guide chemotherapy selection based on tumor genetics and patient factors, maximizing efficacy while minimizing toxicity. Psychiatric care benefits from predictions of antidepressant response, helping clinicians select optimal medications and avoid the trial-and-error approach that prolongs patient suffering.
Population health management utilizes predictive analytics to identify communities and demographic groups at elevated risk for specific health conditions, enabling targeted public health interventions. Machine learning analysis of social determinants, environmental factors, and health utilization patterns reveals disparities and guides resource allocation to underserved populations. As predictive models incorporate increasingly comprehensive data and sophisticated algorithms, their accuracy and clinical utility continue to expand, making predictive analytics an indispensable tool in modern healthcare delivery.
Personalized Treatment Plans and Precision Medicine

Precision medicine, enabled by machine learning, represents a fundamental shift from the traditional one-size-fits-all approach to treatment toward individualized therapies tailored to each patient’s unique characteristics. Machine learning algorithms integrate diverse data sources, including genomic information, electronic health records, lifestyle factors, environmental exposures, and treatment responses to develop personalized treatment plans that optimize outcomes while minimizing adverse effects. This approach recognizes that patients with similar diagnoses may require vastly different therapeutic strategies based on their biological makeup and circumstances.
Pharmacogenomics, the study of how genes affect drug response, has been revolutionized by machine learning analysis. AI systems can predict which medications will be most effective and safe for individual patients based on their genetic profiles, preventing adverse drug reactions and treatment failures. For example, machine learning models guide warfarin dosing by analyzing genetic variants that influence drug metabolism, reducing bleeding complications, and improving anticoagulation control. Similarly, oncology treatments increasingly rely on tumor genetic profiling analyzed by AI algorithms to select targeted therapies with the highest likelihood of success.
Cancer treatment has been particularly transformed by precision medicine approaches. Machine learning analyzes tumor genomic sequencing data to identify actionable mutations and predict responses to immunotherapy, targeted therapy, and conventional chemotherapy. AI-powered clinical decision support systems match patients to appropriate clinical trials based on their tumor characteristics and treatment history, expanding access to cutting-edge therapies. Radiation therapy planning utilizes machine learning to optimize beam angles and dosing, maximizing tumor destruction while sparing healthy tissue.
Chronic disease management benefits from machine learning-based personalization of treatment regimens. Diabetes care platforms use AI algorithms to analyze continuous glucose monitoring data, insulin dosing, dietary intake, and physical activity to provide real-time recommendations for insulin adjustments. These systems learn individual patient patterns and responses over time, continuously refining their recommendations to achieve optimal glycemic control. Similarly, hypertension management employs machine learning to personalize medication selection and dosing based on patient characteristics, comorbidities, and response patterns.
Mental health treatment increasingly leverages machine learning for treatment personalization. Predictive models analyze patient demographics, symptom profiles, treatment histories, and genetic markers to forecast responses to different antidepressant medications and psychotherapy approaches. This evidence-based guidance helps clinicians select optimal treatments more quickly, reducing the prolonged trial-and-error periods that characterize traditional psychiatric care. Natural language processing of therapy session transcripts and patient-reported outcomes enables real-time assessment of treatment progress and early detection of clinical deterioration.
Rare disease management has been revolutionized by machine learning’s ability to analyze complex genetic and clinical data to identify disease-causing mutations and guide treatment selection. AI systems match patients with ultra-rare conditions to appropriate therapies, clinical trials, and support resources that would be nearly impossible to identify through conventional means. As databases of genetic variants and treatment outcomes grow, machine learning models become increasingly effective at guiding personalized treatment for even the rarest conditions, offering hope to patient populations previously lacking evidence-based therapeutic options.
Medical Imaging and Computer Vision Applications
Medical imaging analysis represents one of the most mature and impactful applications of machine learning in healthcare, with computer vision algorithms achieving diagnostic accuracy that rivals or exceeds human specialists in many domains. Deep learning models, particularly convolutional neural networks, excel at detecting patterns in radiological images, pathology slides, and other visual medical data, providing rapid, consistent, and highly accurate interpretations that augment physician capabilities and improve patient outcomes.
Radiology has been fundamentally transformed by AI-powered image analysis. Machine learning algorithms trained on millions of chest X-rays can detect pneumonia, tuberculosis, lung nodules, and other pulmonary abnormalities with radiologist-level accuracy. Deep learning systems analyze CT scans to identify brain hemorrhages, strokes, and traumatic injuries, prioritizing critical cases for urgent radiologist review and expediting treatment initiation. In mammography, AI algorithms serve as a second reader, identifying suspicious lesions that might be overlooked in initial screenings and reducing false negative rates in breast cancer detection.
Pathology is experiencing a digital revolution driven by machine learning analysis of whole-slide images. AI systems examine tissue samples for cancerous cells, grade tumor aggressiveness, and predict treatment responses with remarkable precision. Deep learning models can distinguish between different cancer subtypes, identify prognostic markers, and detect patterns invisible to human pathologists, such as subtle cellular features associated with specific genetic mutations. This AI-assisted pathology improves diagnostic consistency, reduces interpretation time, and enables remote expertise sharing to underserved areas.
Ophthalmology has pioneered the clinical deployment of machine learning diagnostic systems. AI algorithms screen retinal photographs for diabetic retinopathy, age-related macular degeneration, and glaucoma, enabling early detection in primary care settings without requiring ophthalmologist evaluation for every patient. Deep learning models analyze optical coherence tomography (OCT) images to guide treatment decisions for retinal diseases, predicting progression and response to therapies. These systems have been particularly impactful in expanding access to specialized eye care in resource-limited settings.
Dermatology benefits from computer vision applications that analyze skin lesion photographs to distinguish benign moles from melanomas and other skin cancers. Machine learning models trained on diverse patient populations and lesion types achieve diagnostic accuracy comparable to board-certified dermatologists, making skin cancer screening more accessible through smartphone applications and telemedicine platforms. AI systems also assist in monitoring chronic skin conditions like psoriasis and eczema, tracking disease activity and treatment responses over time.
Cardiology imaging employs machine learning to automate measurements and assessments from echocardiograms, cardiac MRI, and coronary angiography. AI algorithms calculate ejection fraction, assess valve function, quantify myocardial scar tissue, and identify coronary artery stenoses with high accuracy and reproducibility. These automated analyses save clinician time, reduce inter-observer variability, and enable rapid triage of abnormal studies requiring urgent intervention. Deep learning applied to cardiac imaging data can predict future cardiovascular events, guiding preventive interventions.
The integration of machine learning into medical imaging workflows addresses critical challenges, including radiologist shortages, interpretation variability, and the need for rapid turnaround times in emergency settings. AI-powered triage systems prioritize critical findings, ensuring that patients with life-threatening conditions receive immediate attention. As computer vision technology continues advancing and regulatory frameworks mature, machine learning in medical imaging will become increasingly integrated into routine clinical practice, enhancing diagnostic accuracy and efficiency across all medical specialties.
Drug Discovery and Development
Drug discovery and development, traditionally a lengthy and expensive process requiring over a decade and billions of dollars to bring a new medication to market, is being revolutionized by machine learning technologies. AI algorithms accelerate every stage of pharmaceutical development, from target identification and compound screening to clinical trial design and patient recruitment, promising to reduce timelines and costs while increasing success rates. This transformation addresses the pharmaceutical industry’s productivity crisis and expedites the delivery of life-saving therapies to patients.
Target identification, the process of determining which biological molecules to target with new drugs, benefits immensely from machine learning analysis of genomic, proteomic, and metabolomic data. AI systems analyze disease mechanisms, genetic associations, and molecular pathways to identify promising drug targets with a high likelihood of clinical success. Machine learning models predict target druggability, potential off-target effects, and optimal patient populations, focusing research efforts on targets most likely to yield effective therapies. This approach has been particularly valuable in complex diseases like cancer, neurodegenerative disorders, and autoimmune conditions.
Compound screening and optimization, traditionally requiring years of laboratory experimentation, are dramatically accelerated by machine learning. AI algorithms predict how potential drug molecules will interact with target proteins, assessing binding affinity, specificity, and pharmacological properties computationally before laboratory synthesis. Deep learning models trained on millions of known compound-protein interactions can screen billions of virtual compounds in days, identifying promising candidates for further development. Generative AI designs entirely novel molecules optimized for desired properties, expanding the chemical space available for drug discovery.
Preclinical development employs machine learning to predict drug toxicity, pharmacokinetics, and efficacy in animal models and human cells. AI systems analyze structural features of compounds to forecast potential adverse effects, metabolism pathways, and dosing requirements, reducing the failure rate in later development stages. Machine learning models integrate data from diverse preclinical assays to provide comprehensive safety and efficacy profiles, guiding optimization of lead compounds before expensive clinical testing begins.
Clinical trial design and execution are being transformed by AI-powered analytics. Machine learning algorithms optimize trial protocols, including patient selection criteria, dosing regimens, endpoint definitions, and statistical analysis plans, maximizing the likelihood of demonstrating efficacy while minimizing patient risk. Predictive models identify patients most likely to respond to investigational therapies, enabling enrichment strategies that improve trial success rates. Natural language processing of electronic health records facilitates patient recruitment by identifying eligible individuals across healthcare systems, accelerating enrollment timelines.
Real-world evidence generation benefits from machine learning analysis of post-market drug performance. AI systems analyze electronic health records, insurance claims, and patient registries to identify rare adverse events, assess long-term efficacy, and discover new therapeutic indications for existing medications. This repurposing of approved drugs for new uses, accelerated by machine learning, provides rapid access to treatments for conditions lacking therapeutic options. The COVID-19 pandemic demonstrated this potential when AI-driven drug repurposing efforts identified existing medications with antiviral properties for emergency use.
As machine learning becomes increasingly integrated into pharmaceutical research and development, the traditional linear drug development paradigm is giving way to a more iterative, data-driven approach. AI systems continuously learn from experimental results, clinical data, and real-world outcomes, refining predictions and guiding decision-making throughout the drug lifecycle. This transformation promises to increase the productivity of pharmaceutical research, reduce development costs, and accelerate the delivery of innovative therapies to patients suffering from currently untreatable conditions.
Electronic Health Records Management and Optimization
Electronic health records (EHR) serve as the digital backbone of modern healthcare, containing comprehensive patient information that, when effectively leveraged through machine learning, can transform clinical decision-making, operational efficiency, and population health management. However, EHR systems also present challenges, including data fragmentation, interoperability issues, and clinician burnout from documentation burden. Machine learning technologies address these challenges while unlocking the immense value contained within EHR data to improve patient care and system performance.
Clinical documentation, one of the most time-consuming aspects of modern medical practice, is being revolutionized by AI-powered solutions. Natural language processing technologies convert physician-patient conversations into structured clinical notes, reducing documentation time and allowing clinicians to focus on direct patient care. Ambient AI scribes listen to clinical encounters and automatically generate comprehensive visit notes, including chief complaint, history of present illness, physical examination findings, assessment, and treatment plan. These systems learn individual physician preferences and specialty-specific documentation requirements, producing notes that require minimal editing before finalization.
Data extraction and structuring from unstructured EHR text represents another critical application of machine learning. Clinical notes, discharge summaries, and radiology reports contain rich information that exists as free text rather than structured data fields. Natural language processing algorithms extract relevant clinical information, including diagnoses, medications, procedures, and outcomes from these narratives, making the information searchable, analyzable, and actionable. This structured data enables population health analytics, quality measurement, and clinical decision support that would be impossible with unstructured text alone.
Clinical decision support powered by machine learning leverages EHR data to provide real-time guidance at the point of care. AI systems analyze patient histories, current medications, laboratory results, and clinical guidelines to alert physicians to potential drug interactions, contraindications, and evidence-based treatment recommendations. Predictive analytics integrated into EHR workflows flag patients at risk for adverse events like sepsis or cardiac arrest, prompting early interventions. These intelligent alerts are tuned to minimize false positives that cause alert fatigue, focusing the physician’s attention on truly actionable warnings.
Medication management benefits significantly from machine learning analysis of EHR data. AI algorithms identify medication errors, including incorrect dosing, duplicate therapies, and inappropriate drug combinations, before prescriptions are dispensed. Predictive models assess patient-specific factors to recommend optimal medication choices and doses, accounting for kidney function, drug interactions, genetic factors, and previous treatment responses. Machine learning also supports medication reconciliation during care transitions, reducing discrepancies that can lead to adverse drug events.
Quality improvement and compliance efforts leverage machine learning to analyze EHR data for adherence to clinical guidelines, identification of care gaps, and detection of safety events. AI systems automatically calculate quality metrics, identify patients overdue for preventive services, and generate reports for regulatory submissions. Natural language processing reviews clinical documentation for completeness and coding accuracy, improving revenue cycle management and reducing compliance risks. As interoperability standards mature and EHR systems become increasingly integrated with machine learning capabilities, the potential for AI to optimize healthcare delivery through better information management continues to expand.
Remote Patient Monitoring and Wearable Technology

Remote patient monitoring enabled by wearable devices and machine learning represents a paradigm shift from episodic, facility-based care to continuous, home-based health management. Wearable technology, including smartwatches, continuous glucose monitors, cardiac monitors, and activity trackers, generates streams of physiological data that, when analyzed by AI algorithms, provide unprecedented insights into patient health status and enable early intervention before conditions deteriorate. This approach is particularly valuable for chronic disease management and post-acute care monitoring.
Cardiovascular monitoring has been transformed by wearable devices with machine learning capabilities. Smartwatches equipped with electrocardiogram (ECG) sensors continuously monitor heart rhythm, detecting atrial fibrillation, bradycardia, and tachycardia in real-time. AI algorithms distinguish true arrhythmias from artifacts and physiological variations, alerting patients and physicians only when clinically significant events occur. Machine learning models analyze heart rate variability, activity patterns, and sleep data to assess cardiovascular health trends and predict adverse events like heart failure exacerbations days before symptoms manifest.
Diabetes management benefits immensely from continuous glucose monitoring (CGM) integrated with machine learning analytics. AI-powered systems predict hypoglycemic and hyperglycemic episodes 30-60 minutes in advance based on glucose trends, food intake, insulin administration, and physical activity, alerting patients to take preventive action. Machine learning algorithms optimize insulin dosing recommendations, learning individual response patterns to create increasingly personalized guidance. Integration with automated insulin delivery systems creates closed-loop artificial pancreas technology that dramatically improves glycemic control while reducing patient burden.
Respiratory disease monitoring employs wearable sensors that track breathing patterns, oxygen saturation, and activity levels. Machine learning analysis identifies exacerbation patterns in conditions like chronic obstructive pulmonary disease (COPD) and asthma, enabling early intervention before hospitalizations become necessary. During the COVID-19 pandemic, remote monitoring platforms demonstrated their value for managing patients at home, detecting clinical deterioration requiring hospitalization while avoiding unnecessary emergency department visits.
Neurological condition monitoring leverages wearable accelerometers and motion sensors to track symptom progression and treatment responses. Parkinson’s disease patients benefit from continuous monitoring of tremor severity, gait disturbances, and medication effectiveness throughout daily activities rather than brief clinic visits. Machine learning identifies patterns in symptom fluctuations and optimizes medication timing. Epilepsy patients use wearable devices with AI algorithms that detect seizures and alert caregivers, providing safety monitoring and objective seizure diaries to guide treatment adjustments.
Post-surgical monitoring and chronic wound care employ wearable sensors and machine learning to track healing progress and detect complications early. Smart bandages with embedded sensors monitor temperature, moisture, and other indicators of infection, alerting care teams to intervene before serious complications develop. Post-discharge monitoring following major surgeries tracks vital signs, activity levels, and patient-reported symptoms, identifying patients requiring readmission while providing reassurance to those recovering normally.
The integration of remote patient monitoring data with electronic health records creates comprehensive longitudinal health profiles that enable more informed clinical decision-making. Machine learning synthesizes information from multiple wearable devices, clinical encounters, and patient-reported outcomes to provide holistic assessments of health status and treatment effectiveness. As sensor technology advances, costs decrease, and reimbursement models evolve to support remote monitoring, these AI-powered solutions will become standard components of chronic disease management and post-acute care, improving outcomes while reducing healthcare costs.
Challenges and Ethical Considerations
Despite the transformative potential of machine learning in healthcare, significant challenges and ethical considerations must be addressed to ensure responsible implementation that benefits patients while minimizing risks. Data privacy, algorithmic bias, model interpretability, regulatory compliance, and integration into clinical workflows represent critical barriers that require thoughtful solutions from technologists, clinicians, policymakers, and ethicists working collaboratively.
Data privacy and security concerns are paramount when implementing machine learning systems that process sensitive health information. Electronic health records, genomic data, and information from wearable devices contain intimate details about individuals that must be protected from unauthorized access, breaches, and misuse. Machine learning models trained on patient data risk privacy violations through membership inference attacks, where adversaries determine whether specific individuals’ data was used in training. Federated learning and differential privacy techniques offer promising approaches to train models while preserving patient confidentiality, but widespread adoption remains limited. Healthcare organizations must implement robust security measures, encryption protocols, and access controls to protect machine learning infrastructure from cyber threats.
Algorithmic bias represents a critical ethical challenge that can perpetuate and amplify healthcare disparities. Machine learning models trained on historically biased data or non-representative populations may perform poorly for underrepresented demographic groups, leading to misdiagnosis, inappropriate treatment recommendations, and unequal care quality. For example, AI systems trained primarily on data from one racial or ethnic group may be less accurate when applied to other populations. Addressing algorithmic bias requires diverse training datasets, rigorous validation across demographic subgroups, and ongoing monitoring of model performance in real-world clinical settings. Transparency in model development and deployment helps identify and mitigate bias before it harms patients.
Model interpretability poses challenges for clinical adoption of machine learning, particularly deep learning models that function as “black boxes” with opaque decision-making processes. Clinicians require an explanation of why AI systems reach specific conclusions to trust recommendations and explain them to patients. Explainable AI (XAI) techniques, including attention maps, feature importance scores, and counterfactual explanations, help elucidate model reasoning, but balancing interpretability with predictive accuracy remains challenging. Regulatory agencies increasingly require documentation of model logic and validation evidence before approving AI-powered medical devices.
Regulatory oversight of machine learning in healthcare lags behind technological advancement, creating uncertainty about approval pathways, safety standards, and post-market surveillance requirements. Traditional medical device regulations were designed for static products rather than AI systems that learn and evolve. Regulatory agencies worldwide are developing adaptive frameworks for AI-based medical devices, but harmonization across jurisdictions and clarity about evidentiary standards remain incomplete. Healthcare organizations face challenges in determining which machine learning applications require regulatory approval versus those that constitute clinical decision support tools exempt from device regulations.
Clinical integration challenges include workflow disruption, alert fatigue, and resistance to change among healthcare professionals. AI systems that generate excessive false alerts or require substantial additional effort undermine clinical efficiency and face rejection by users. Successful implementation requires careful user experience design, integration with existing EHR systems, and involvement of frontline clinicians in development and testing. Training healthcare professionals to understand machine learning capabilities and limitations ensures appropriate use and prevents over-reliance on AI recommendations.
Liability and accountability questions arise when AI-powered clinical decisions lead to adverse outcomes. Determining responsibility among algorithm developers, healthcare institutions, and individual clinicians requires new legal and ethical frameworks. Professional liability insurance policies may not clearly cover AI-assisted care, creating financial risks for early adopters. Establishing transparent documentation of machine learning system performance, limitations, and appropriate use cases helps clarify accountability and protect patients.
Addressing these challenges requires multi-stakeholder collaboration, evidence-based policymaking, and commitment to ethical principles, including beneficence, non-maleficence, autonomy, and justice. As machine learning becomes increasingly embedded in healthcare delivery, ongoing vigilance, evaluation, and course correction will ensure these powerful technologies serve all patients equitably and safely.
Future Trends and Innovations
The future of machine learning in healthcare promises even more transformative innovations as technology advances, datasets expand, and clinical integration deepens. Emerging trends, including multimodal AI, edge computing, quantum machine learning, and increasingly sophisticated autonomous systems, will expand the boundaries of what’s possible in patient care, drug discovery, and health system optimization. These trajectories help healthcare organizations and policymakers prepare for the coming waves of innovation.
Multimodal AI systems that integrate diverse data types, including medical images, electronic health records, genomic sequences, wearable sensor data, and environmental information, will provide more comprehensive patient assessments than models analyzing single data modalities. These systems will capture the complexity of human health by synthesizing information across biological scales and time periods, enabling more accurate predictions and personalized interventions. Foundation models trained on vast amounts of medical data across specialties will serve as starting points for specific clinical applications, reducing development time and improving performance.
Edge computing and on-device machine learning will enable real-time analysis of patient data without requiring cloud connectivity, addressing latency, privacy, and reliability concerns. Wearable devices with embedded AI chips will detect health emergencies like cardiac arrest or seizures within seconds, triggering immediate alerts and interventions. Medical imaging equipment with integrated machine learning will provide preliminary interpretations instantly, streamlining workflow and expediting care. This distributed intelligence reduces dependence on centralized computing infrastructure and enhances system resilience.
Quantum machine learning, though still in early stages, promises exponential acceleration of computationally intensive tasks, including molecular modeling for drug discovery, optimization of treatment protocols, and analysis of massive genomic datasets. Quantum computers’ ability to explore vast solution spaces simultaneously could revolutionize personalized medicine by identifying optimal combinations of therapies from millions of possibilities. As quantum hardware matures and becomes more accessible, pharmaceutical companies and research institutions will increasingly leverage these capabilities.
Autonomous surgical systems guided by machine learning will assist or independently perform certain procedures with superhuman precision and consistency. Robotic surgery platforms already provide tremor filtration and motion scaling, but future systems will incorporate real-time tissue analysis, anatomical recognition, and adaptive planning based on intraoperative findings. AI-guided surgery will be particularly valuable in microsurgical procedures, delicate neurosurgery, and minimally invasive interventions where precision is paramount.
Digital twins, virtual replicas of individual patients built from comprehensive physiological and molecular data, will enable simulation of treatment responses before actual administration. Machine learning will continuously update these models based on real-time patient data, enabling dynamic treatment optimization throughout disease courses. Clinical trials will increasingly employ digital twins to simulate patient responses, reducing the need for large control groups and accelerating development timelines.
Ambient intelligence in healthcare facilities will create environments that continuously monitor patient status, anticipate needs, and optimize conditions for healing. Machine learning systems will analyze data from room sensors, bedside monitors, and electronic health records to detect subtle changes in patient condition, adjust environmental factors like lighting and temperature, and alert staff to potential issues before they become critical. This smart hospital infrastructure will reduce adverse events, improve patient experience, and enhance operational efficiency.
Blockchain integration with machine learning systems will enhance data security, interoperability, and patient control over health information. Distributed ledger technology can create immutable audit trails of AI decisions, ensuring accountability and transparency. Patients will control access to their health data while enabling machine learning models to be trained on decentralized datasets without compromising privacy. Smart contracts will automate consent management, data sharing agreements, and compensation for individuals contributing data to research.
Conversational AI and natural language processing will evolve into sophisticated virtual health assistants capable of conducting preliminary consultations, providing health education, managing chronic conditions, and offering mental health support. These AI assistants will understand context, emotion, and cultural nuances, providing personalized guidance that adapts to individual patient needs and preferences. Integration with wearable devices and electronic health records will enable these systems to provide comprehensive health coaching and early intervention recommendations.
As these innovations mature and converge, machine learning will become increasingly invisible yet indispensable in healthcare delivery, seamlessly integrated into clinical workflows and patient experiences. The next decade will witness transformation not just in specific applications but in the fundamental structure of healthcare systems, shifting from reactive, episodic care to proactive, continuous health optimization powered by artificial intelligence and machine learning.
More Read: How to Build Your First Machine Learning Model Step by Step
Conclusion
Machine learning in healthcare represents a transformative force that is fundamentally reshaping patient care, clinical decision-making, and health system operations. From early disease detection and predictive analytics to personalized treatment plans and drug discovery, AI-powered solutions are improving diagnostic accuracy, optimizing therapies, and enabling proactive interventions that save lives and reduce suffering. Medical imaging analysis, electronic health records management, and remote patient monitoring demonstrate the breadth of applications where machine learning enhances both clinical outcomes and operational efficiency.
Despite significant challenges, including data privacy, algorithmic bias, regulatory uncertainty, and integration complexities, the trajectory is clear: artificial intelligence and machine learning will become indispensable components of modern healthcare delivery. As technology advances and adoption accelerates, the promise of precision medicine, accessible specialist-level care, and truly personalized health management moves from aspiration to reality.
The successful realization of this potential requires continued collaboration among technologists, clinicians, policymakers, and patients to ensure that machine learning innovations benefit all populations equitably while upholding the highest standards of safety, privacy, and ethical practice. The healthcare transformation powered by machine learning is not merely augmenting existing practices but fundamentally reimagining what is possible in the pursuit of human health and wellbeing.